How your brain is wired to just say ‘yes’ to opioids
- Written by Paul R. Sanberg, Senior Vice President for Research, Innovation & Knowledge Enterprise, University of South Florida
The mid-1980s was the era of cocaine and marijuana, when “Just Say No”[1] was the centerpiece of the war on drugs and the government’s efforts to stem drug use and addiction. Since then, prescription opioids[2] have become the nation’s drug scourge. The idea that mere willpower can fight this public health emergency is not only outdated, it’s scientifically misguided.
Medical history tells us that almost as long as there have been opioids – their use dates back to the third century[3] – there have been opioid addicts.
Thirty years ago, I was a research scientist focused on addiction when I was asked to co-author a volume on prescription narcotics for the “Encyclopedia of Psychoactive Drugs.[4]” I wrote the same assessment of opioid abuse then that I would write today: For many people, opioids are substances their brains are wired to crave in ways that make personal resolve nearly impossible.
Your brain on opioids
Our understanding of the human brain’s mechanisms make a compelling argument for a national research effort to develop non-opioid painkillers and new medical devices to treat chronic pain, which remains the nation’s number one cause of disability.[5] The good, if somewhat little noticed, news is that there is meaningful action on this front led by the National Institutes of Health, which is working in conjunction with pharmaceutical companies to develop nonaddictive, non-opioid pain killers[6] that might finally end our somewhat tortured dependence on this formidable drug.
Brain scientists have known for decades that opioids are complex and difficult substances to manage when it comes to addiction. The National Institute on Drug Abuse reports[7] that more than 20 percent of the patients prescribed opioids for chronic pain misuse them, and between 8 and 12 percent of those who use prescription opioids develop a use disorder.
Given how addictive these drugs are, doctors should have foreseen the looming danger of prescription opioids long before their use was liberalized for non-cancer related pain in the 1990s. Opioid abuse has instead ballooned over the last decade. In 2014, federal officials estimated nearly 2 million people[8] in the United States suffer from substance use disorders related to prescription opioid pain medicines. Each day, more than 1,000 people are treated[9] in emergency rooms for misusing prescription opioids, the CDC reports.
The reason? Many people’s brains are wired to want this drug.
How opioids affect the brain
The simplified explanation of this complex brain science is this: When opioids enter the brain, they bind to receptors known as μ (mu) opioid receptors on brain cells, or neurons. These receptors stimulate the “reward center” of the brain. This occurs in a part of the brain known as the ventral tegmental area[10], which results in the release of the neurotransmitter chemical dopamine. Over time, those receptors become less sensitive, and more of the drug is needed to stimulate the reward center.
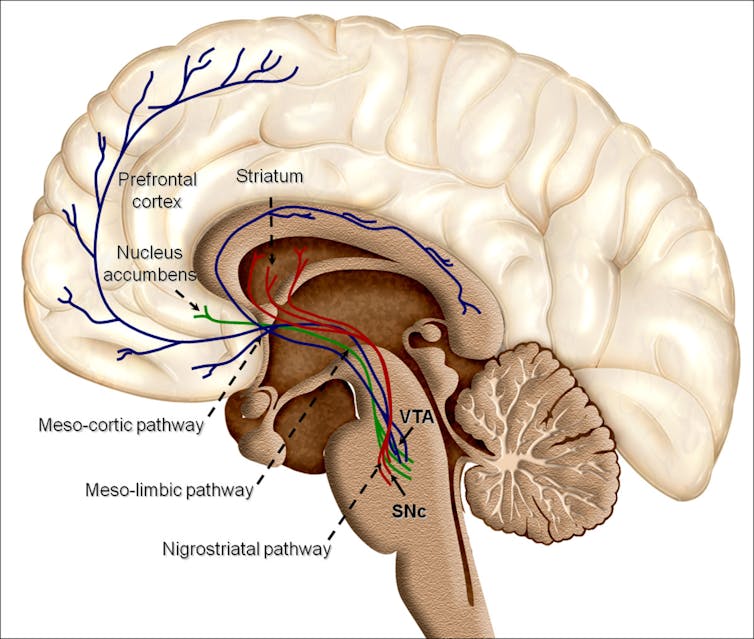 Overview of reward structures in the human brain.
By Oscar Arias-Carrión, Maria Stamelou, Eric Murillo-Rodríguez, Manuel Menéndez-González and Ernst Pöppel./Wikimedia.org, CC BY-SA[11][12]
Overview of reward structures in the human brain.
By Oscar Arias-Carrión, Maria Stamelou, Eric Murillo-Rodríguez, Manuel Menéndez-González and Ernst Pöppel./Wikimedia.org, CC BY-SA[11][12]
A brain that has become dependent on opioids can produce a strong desire to avoid the very real physical pain of withdrawal[13]. When opioids are absent in the body after the person has become dependent, another neurotransmitter called noradrenaline is produced in excess. Excessive production of NA results in withdrawal symptoms[14] that include shaking, tremors, anxiety, muscle cramps, and other uncomfortable and painful physiological responses. Users self-correct this brain chemistry by continuing to take the drug to stimulate dopamine production in their brain.
Our learning and memory processes also become engaged in addiction to a substance. A few brain areas are involved in the continued use of opioids after the pleasure factor has subsided and the person is still using the drug in order to avoid withdrawal. These areas include the paraventricular nucleus of the thalamus[15], bed nucleus of the stria terminalis[16], the amygdala and other areas. A user’s brain can literally create a strong aversion to opioid withdrawal and compel them to keep using even if they know they are nearing an overdose.
The research community responds
Brain science is only one part of an addiction problem, but, I believe an important one deserving of more consideration than we’ve shown in past drug abuse crises. NIH Director Francis S. Collins[17] has recognized this in his leadership of the medical and scientific response to the opioid use epidemic.
The NIH is taking important steps[18] in building a public-private partnership that will seek scientific solutions to the opioid crisis, including the development of non-opioid painkillers. Collins has committed his agency’s resources in this quest, including implementing the Fast Track and Breakthrough Therapy designations that exist to facilitate development and expedite review of products that address an unmet medical need. The agency is calling for more emphasis on non-drug alternatives[19] for pain, such as medical devices that can deliver more localized analgesia.
Expediency and proper funding of this effort is critical to get effective alternatives to those who need it most – the people fully intending to “Just Say No” but whose brains will fight them every step of the way.
References
- ^ “Just Say No” (www.nbcnews.com)
- ^ prescription opioids (www.cdc.gov)
- ^ third century (www.ncbi.nlm.nih.gov)
- ^ “Encyclopedia of Psychoactive Drugs. (www.librarything.com)
- ^ the nation’s number one cause of disability. (report.nih.gov)
- ^ to develop nonaddictive, non-opioid pain killers (www.ncbi.nlm.nih.gov)
- ^ reports (www.drugabuse.gov)
- ^ federal officials estimated nearly 2 million people (www.cdc.gov)
- ^ 1,000 people are treated (www.cdc.gov)
- ^ ventral tegmental area (www.ncbi.nlm.nih.gov)
- ^ By Oscar Arias-Carrión, Maria Stamelou, Eric Murillo-Rodríguez, Manuel Menéndez-González and Ernst Pöppel./Wikimedia.org (commons.wikimedia.org)
- ^ CC BY-SA (creativecommons.org)
- ^ withdrawal (medlineplus.gov)
- ^ withdrawal symptoms (www.els.net)
- ^ paraventricular nucleus of the thalamus (www.ncbi.nlm.nih.gov)
- ^ bed nucleus of the stria terminalis (www.ncbi.nlm.nih.gov)
- ^ Francis S. Collins (directorsblog.nih.gov)
- ^ NIH is taking important steps (www.nih.gov)
- ^ non-drug alternatives (www.nih.gov)
Authors: Paul R. Sanberg, Senior Vice President for Research, Innovation & Knowledge Enterprise, University of South Florida
Read more http://theconversation.com/how-your-brain-is-wired-to-just-say-yes-to-opioids-90805

