Doctors treating trans youth grapple with uncertainty, lack of training
- Written by stef m. shuster, Assistant Professor of Sociology, Michigan State University
Last month, the Arkansas Senate passed legislation prohibiting medical providers from offering gender-affirming hormones or surgeries to trans youth.
If you were to read the bill – titled the Save Adolescents From Experimentation Act[1] – you might think the law was protecting children from physicians like Josef Mengele[2], the Nazi doctor who experimented on Jewish people.
“It is of grave concern to the General Assembly,” the text reads, that trans youth are being allowed “to be subjects of irreversible and drastic” treatments “despite the lack of studies showing that the benefits of such extreme interventions outweigh the risks.”
This language is at odds with the growing evidence that blocking people from accessing gender-affirming care creates increased risks[3] for social isolation, suicide ideation and depression. Withholding puberty blockers from trans and nonbinary youth has also been found to negatively affect mental health[4].
However, the hyperbolic language and imagery of brutal experimentation prevents medical providers from honestly confronting the various issues that do exist within the field. The punitive nature of the legislation – in which doctors can lose their licenses – further thwarts these efforts.
As I discuss in my new book, “Trans Medicine[5],” little scientific evidence exists to support the use of current trans medical treatments, therapy or decision-making that meets evidence-based standards[6]. Randomized controlled trials have yet to be conducted.
For this reason, providers often have trepidation about working with trans people, even if they recognize it is in the best interests of their patients to do so.
A history of resistance
Pointing out the lack of evidence[7] in this medical field is nothing new.
Providers of trans medicine have dealt with accusations of engaging in unnecessary – even immoral – experimentation and “quackery” since the mid-20th century. Many of these charges came from other doctors.
For example, in a letter to a colleague, Harry Benjamin, a well-known endocrinologist who worked during the 1950s, wrote, “I can’t tell you how many of my fellows have called me aside for a heart-to-heart talk on this business of working with transsexuals. They worried about the gossip surrounding me and my office as a result of this type of work.”
As Benjamin suggested – and as the historical record reflected[8] – scandal overwhelmed those providers willing to offer hormone therapy for trans people. After all, an individual who requested to change their gender presentation was understood as having a mental illness, best addressed by long-term therapy.
The medical establishment has typically responded to such charges of quackery, even from other doctors[9] by touting their specialized training, credentials and skills to deal with disease and illness.
But for over 70 years, physicians and therapists who work with trans clients, young and old, have nonetheless been haunted by a very basic question: How might someone who is trained to manage illness and disease “treat” someone’s gender identity, which is neither an illness nor a disease?
Swimming in doubt
The question seems simple. But it reflects the ambivalence many doctors and therapists have toward trying to apply standard medical or therapeutic models to gender identities.
Take Margaret, a family care physician who had been working for about five years in trans medicine before we met one afternoon to discuss her experiences. (The names used in my research are pseudonyms.)
“I don’t always know if I am doing the right thing when I work with trans patients,” she told me. “I haven’t been trained in this area. So, if I have a patient who has high cholesterol or is a smoker, but wants to start estrogen, what do I do? To not offer estrogen seems harmful because that would help her be able to express her gender that reflects who she is. But what about the health risks? What am I supposed to do?” (There is mixed evidence[10] on the relationship between taking hormones and heightened risks for heart attacks or strokes.)
Health care experts are used to feeling like they have a good foundation of knowledge to make informed decisions, so this can be an uneasy space for doctors like Margaret to work in.
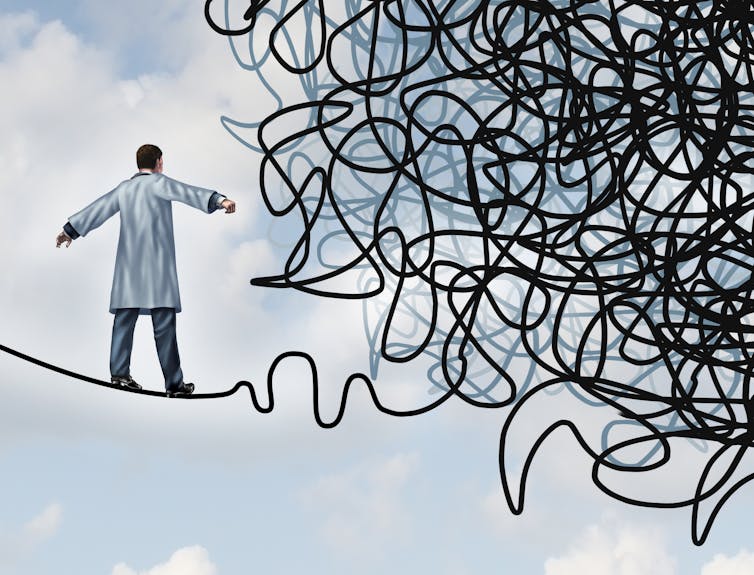 Doctors who treat trans people are often forced to rely on their gut, in lieu of clinical guidelines.
wildpixel via Getty Images[11]
Doctors who treat trans people are often forced to rely on their gut, in lieu of clinical guidelines.
wildpixel via Getty Images[11]
Her experiences are not unique. After I spent time searching in the Kinsey Institute’s archives[12], which house correspondence from mid-20th-century providers, interviewing physicians and therapists across the U.S. who work with trans youth and adults, and observing them at health conferences, it became clear to me that the uncertainty Margaret expressed permeates trans medicine.
Alexis, a social worker I interviewed, told me one of the difficulties working with trans people is that each person is unique – “There is this person and this person and this person,” she explained. Trying to apply a standard model for decision-making onto trans experience is difficult. Trans people have complex ways of understanding their identities. The reason to pursue medical interventions varies from one person to the next.
Not all providers comfortably lean on this flexibility in delivering gender-affirming care or therapy. Speaking before her colleagues at a health care conference, one physician urged them to remember, before starting their patients on hormones, that “what you are looking to get at is to make sure their gender identity is clear and there are no red flags.”
But there are no medical tests to confirm a trans identity. And “red flags” aren’t defined or delineated in any literature or clinical guidelines.
Barriers to understanding
Once doctors have decided to pursue a course of treatment, the science isn’t exactly settled. Part of that has to do with the fact that randomized controlled trials have been implausible, given that only 0.6% of the population[13] identifies as trans or nonbinary.
And physicians like Margaret might feel unqualified because most providers encounter only a single “diversity” day[14] during medical residency programs. This day covers lesbian, gay, bisexual and transgender health care – and, in the process, conflates sexuality and gender.
Furthermore, there are few opportunities for providers to gain formal training in trans medicine or therapy. Clinical guidelines – or cookbooks for medical decision-making[15] – for trans medicine offer providers direction about which steps to take to initiate hormone therapy or surgical interventions. But, they rarely discuss how to work with trans and nonbinary people in gender-affirming ways or how to avoid creating roadblocks for trans people to access care.
Still, important advances have been made.
There is a small, but growing, number of studies published on the efficacy of surgical techniques[16] or the effects of hormone therapy[17]. The providers I interviewed acknowledged these studies help them assess how much of a hormone to prescribe. But these data did little to help providers decide when to initiate, continue, or block access to hormones – or how to interact with trans and nonbinary patients in a supportive and inclusive way.
Support – not punishment – needed
The providers I spoke with insisted that they’re trying to do the best they can. But because of the lack of evidence and clinical experience, providers of trans medicine often lean on gut instinct to help them navigate through the murkiness of this medical field.
This can lead to bias seeping into clinical encounters[18]. Providers of trans medicine may not intentionally be prejudiced against certain trans and nonbinary people. But as I point out in my book, when they rely on gut instinct, classism, racism and homophobia can subtly influence their health decisions.
Trans people who identify as women or men, rather than nonbinary, also have an easier time accessing gender-affirming care. The clinical experience of providers has, until recently, emphasized only people transitioning from woman to man or man to woman[19].
Trans medicine is not exceptional, and how providers work their way through making decisions and offering gender-affirming care reflects how providers operate in most new areas of medicine. The COVID-19 pandemic has shown the difficulty that medicine has responding to widespread uncertainty[20].
[Over 100,000 readers rely on The Conversation’s newsletter to understand the world. Sign up today[21].]
There are viable solutions to the concerns raised by legislators. What if, instead of outright banning providers from offering gender-affirming care, more public funding was provided to support longitudinal studies? What if more opportunities were given to providers to gain formal training?
This, in my view, would go a long way in alleviating the unease they experience over of the state of evidence in this medical field.
References
- ^ the Save Adolescents From Experimentation Act (www.arkleg.state.ar.us)
- ^ Josef Mengele (encyclopedia.ushmm.org)
- ^ creates increased risks (doi.org)
- ^ has also been found to negatively affect mental health (doi.org)
- ^ Trans Medicine (nyupress.org)
- ^ evidence-based standards (www.wpath.org)
- ^ lack of evidence (www.doi.org)
- ^ and as the historical record reflected (www.sealpress.com)
- ^ has typically responded to such charges of quackery, even from other doctors (www.basicbooks.com)
- ^ mixed evidence (doi.org)
- ^ wildpixel via Getty Images (www.gettyimages.com)
- ^ Kinsey Institute’s archives (kinseyinstitute.org)
- ^ only 0.6% of the population (ajph.aphapublications.org)
- ^ a single “diversity” day (doi.org)
- ^ cookbooks for medical decision-making (tupress.temple.edu)
- ^ efficacy of surgical techniques (doi.org)
- ^ hormone therapy (doi.org)
- ^ lead to bias seeping into clinical encounters (doi.org)
- ^ emphasized only people transitioning from woman to man or man to woman (doi.org)
- ^ the difficulty that medicine has responding to widespread uncertainty (www.nature.com)
- ^ Sign up today (theconversation.com)
Authors: stef m. shuster, Assistant Professor of Sociology, Michigan State University

