Rural health care is in crisis – here are 5 innovative ways Biden can help it transform
- Written by Lauren Hughes, State Policy Director, Farley Health Policy Center; Associate Professor of Family Medicine, University of Colorado Anschutz Medical Campus
Rural hospitals have struggled with financial troubles for years. Over the past decade, more than 130 have closed[1], forcing residents to drive farther or delay needed care. Now, the COVID-19 pandemic has many of them wondering whether rural health care systems will survive[2].
Twenty percent[3] of the U.S. population lives in rural America, a region that fuels[4] the country with food and energy. These Americans believe their health care needs have been overlooked[5] or misunderstood by Washington[6] for years.
This crisis is now in the hands of the Biden administration. To revive rural health care, the administration will have to expand its push for diversity[7] to also include rural voices so the needs and priorities of rural Americans aren’t neglected in policy agendas for the next four years.
The solutions rural America needs aren’t just about expanding broadband[8] or insurance coverage[9], both of which are critical to extend telehealth and health care access. Rural health care will have to transform to survive and then thrive[10].
One of the first crucial steps is to ensure that trusted rural health care professionals who intimately understand rural America’s challenges are in positions that empower them to shape federal policies that respect rural culture and context. The announcement of the original 13 experts nominated for the Biden transition team’s COVID-19 Advisory Board[11] raised concerns because they largely reflected the coasts and cities at a time when the pandemic raged in rural areas[12].
As experts in rural health policy[13] and population health[14], we work with rural health professionals on solving these challenges. Here are five creative ways the Biden administration can help.
Rethink how rural health care providers are paid
In 2019, Pennsylvania launched an innovative program[15] to help the state’s struggling rural hospitals by changing how they are paid.
Normally, a hospital bills its patients per service. That can encourage hospitals to focus on elective procedures and new technology that can draw more paying patients, rather than promoting wellness and preventing disease. In small, rural hospitals, the volume of services – and ultimately, payment – can also fluctuate widely throughout the year.
Pennsylvania, working with the Center for Medicare and Medicaid Innovation[16], came up with a new design. The Pennsylvania Rural Health Model[17] pays participating hospitals an annual fixed budget that covers inpatient and outpatient services provided at hospitals.
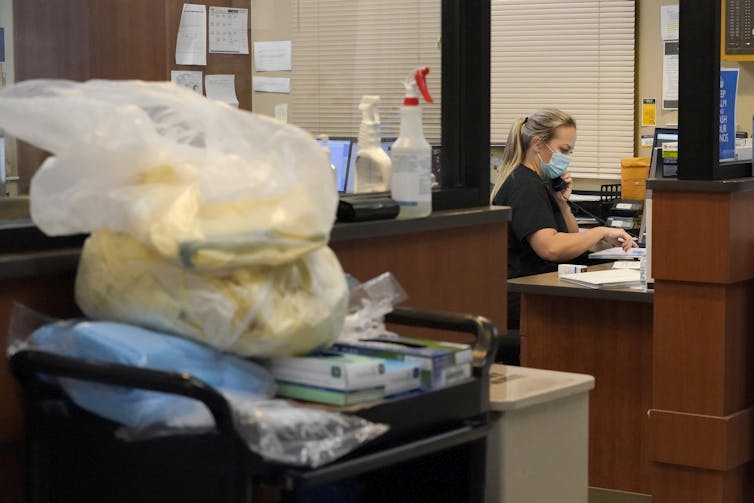
 Many rural residents believe their health care concerns have been ignored by the federal government for years.
Brendan Smialowski/AFP via Getty Images[18]
Many rural residents believe their health care concerns have been ignored by the federal government for years.
Brendan Smialowski/AFP via Getty Images[18]
With a predictable budget, enrolled hospitals can focus on the care their communities need, such as treating addiction, increasing cancer screenings and improving the management of patients’ chronic diseases like diabetes to reduce the need for more expensive acute care. The goal is to reduce costs while improving care[19].
To accelerate rural health care transformation[20] nationwide, the Biden administration could create a dedicated division within the Center for Medicare and Medicaid Innovation focused on rural health. Its mission would be to design and test solutions that address unique problems rural providers face like sparse populations[21] and poorer health status[22]. The administration may have some help coming. Pennsylvania’s former health secretary, Dr. Rachel Levine[23], is now Biden’s nominee for U.S. assistant secretary of health.
Expand mental health services
Mental illness rates are similar in rural and urban America[24], but significant differences exist in access to needed mental health services.
Expanding mental health and addiction services for Medicare and Medicaid recipients and integrating those services with primary care could improve access and reduce stigma[25]. And that could avoid wasteful spending on preventable hospitalizations and medical transfers to larger facilities.
One way to do that is to change Medicare’s lopsided billing rules for mental health care.
Clinics that are designated as either Federally Qualified Health Centers[26] or Rural Health Clinics[27] already receive enhanced payments to provide primary care to Medicare and Medicaid patients. However, the Federally Qualified Health Centers, which are more prevalent in urban areas, can bill[28] for a wider array of mental health and substance use treatment services than the Rural Health Clinics can.
Rural clinics could better address higher rates of behavioral illness[29] and substance misuse[30] if they could fully bill for these services. Changing how telemedicine[31] visits are billed by making them equal to in-person visits would also help rural patients access needed services. To avoid unnecessary costs, these payment changes could be tied to quality measures, such as follow-up appointments after emergency department visits. Nearly a quarter of emergency department visits in the U.S.[32] could be more appropriately managed in outpatient clinics, saving billions of dollars each year.
Build transformational leadership
Rural communities know how to train and recruit physicians through rural medicine rotations[33] and loan repayment[34] programs, but what about hospital administrators?
These are the people who ensure cash-strapped rural hospitals have the supplies and staff they need and can react quickly in a crisis and innovate. Yet, similar pipeline programs for investing in rural health care administration leaders are glaringly absent. Rural America needs leaders with the courage to transform health systems[35], people who can wisely steward resources and think outside the box while improving community health.
 Small hospitals benefit from helping their own staff gain leadership skills.
AP Photo/Jeff Roberson[36]
Small hospitals benefit from helping their own staff gain leadership skills.
AP Photo/Jeff Roberson[36]
Two potential tactics: Rural professionals interested in administrative careers could enroll in innovative master’s programs[37], supported by their employers or through scholarships. The National Health Service Corps[38], which provides doctors with incentives to work in underserved areas, could also adjust its eligibility criteria to repay student loans for health care administration leaders in rural health professional shortage areas[39].
Bring back pregnancy care – in a better way
Fewer than half of rural counties[40] nationwide have hospitals that deliver babies. That, along with difficulty accessing prenatal care, has led to increased childbirth complications[41] like emergency hysterectomies[42] and transferring critically ill newborns.
The new administration could offset costs necessary for Critical Access Hospitals[43] – small, 25-bed hospitals that exist only in rural areas – to deliver babies through special maternity care payments tied to quality outcomes such as increasing breastfeeding rates. These payments would prevent the temptation for small hospitals to grow expensive surgical service lines to cover financial losses commonly associated with offering maternity care[44]. Such payments would also allow rural hospitals to hire dedicated obstetrics nurses[45].
Additional grants through the Patient Centered Outcomes Research Institute[46] could help address rural maternal health disparities and encourage academic medical centers to partner with[47] rural hospitals, clinics and public health departments.
Invest in health-promoting rural infrastructure
Rural communities across the U.S. have witnessed their roads, dams and other infrastructure deteriorate[48] in ways that have endangered health, jobs and their economic competitiveness.
Both the Obama[49] and Trump[50] administrations strengthened rural infrastructure by prioritizing transportation and telecommunication. However, these investments were often viewed as solutions rather than tools for innovation. Rural towns would benefit from infrastructure investments[51] that also encourage healthy behaviors.
[Deep knowledge, daily. Sign up for The Conversation’s newsletter[52].]
Sitka, Alaska[53], winner of the Robert Wood Johnson Foundation Culture of Health Prize, is an example. The town of about 8,600 people has created bike paths, beautified the downtown and built an accessible playground.
The U.S. Department of Agriculture could expand its existing rural infrastructure program[54] by allocating more grant funds for health-promoting activities[55].
Rural America is rich in resourcefulness and diverse in its demographics[56], politics[57] and economics[58]. A transformative approach to revitalizing rural health care would respect its unique assets and culture. With the right commitment to innovation and accountability for achieving equitable outcomes, the Biden[59] administration can build a healthier and more resilient rural America.
References
- ^ 130 have closed (www.shepscenter.unc.edu)
- ^ will survive (www.healthaffairs.org)
- ^ Twenty percent (www.census.gov)
- ^ fuels (healthlaw.org)
- ^ health care needs have been overlooked (doi.org)
- ^ misunderstood by Washington (www.spokesman.com)
- ^ expand its push for diversity (www.politico.com)
- ^ expanding broadband (www.nationalgeographic.com)
- ^ insurance coverage (joebiden.com)
- ^ thrive (cha.com)
- ^ transition team’s COVID-19 Advisory Board (time.com)
- ^ raged in rural areas (dailyyonder.com)
- ^ health policy (medschool.cuanschutz.edu)
- ^ population health (www.siumed.edu)
- ^ Pennsylvania launched an innovative program (www.senatorbaker.com)
- ^ Center for Medicare and Medicaid Innovation (innovation.cms.gov)
- ^ Pennsylvania Rural Health Model (innovation.cms.gov)
- ^ Brendan Smialowski/AFP via Getty Images (www.gettyimages.com)
- ^ goal is to reduce costs while improving care (doi.org)
- ^ rural health care transformation (www.modernhealthcare.com)
- ^ sparse populations (www.cms.gov)
- ^ poorer health status (www.cdc.gov)
- ^ Dr. Rachel Levine (www.npr.org)
- ^ Mental illness rates are similar in rural and urban America (www.ruralhealthinfo.org)
- ^ improve access and reduce stigma (doi.org)
- ^ Federally Qualified Health Centers (www.hrsa.gov)
- ^ Rural Health Clinics (www.cms.gov)
- ^ can bill (www.hrsa.gov)
- ^ behavioral illness (www.ruralhealthresearch.org)
- ^ substance misuse (www.ruralhealthinfo.org)
- ^ telemedicine (www.cms.gov)
- ^ emergency department visits in the U.S. (www.ahrq.gov)
- ^ rural medicine rotations (www.aamc.org)
- ^ loan repayment (www.ruralhealthinfo.org)
- ^ courage to transform health systems (www.astho.org)
- ^ AP Photo/Jeff Roberson (newsroom.ap.org)
- ^ innovative master’s programs (mhcds.dartmouth.edu)
- ^ National Health Service Corps (nhsc.hrsa.gov)
- ^ health professional shortage areas (bhw.hrsa.gov)
- ^ Fewer than half of rural counties (www.hrsa.gov)
- ^ childbirth complications (3pea7g1qp8f3t9ooe3z3npx1-wpengine.netdna-ssl.com)
- ^ emergency hysterectomies (labblog.uofmhealth.org)
- ^ Critical Access Hospitals (www.ruralhealthinfo.org)
- ^ commonly associated with offering maternity care (www.healthleadersmedia.com)
- ^ dedicated obstetrics nurses (pubmed.ncbi.nlm.nih.gov)
- ^ Patient Centered Outcomes Research Institute (www.pcori.org)
- ^ to partner with (www.politico.com)
- ^ infrastructure deteriorate (rebuildrural.com)
- ^ Obama (obamawhitehouse.archives.gov)
- ^ Trump (www.whitehouse.gov)
- ^ infrastructure investments (www.brookings.edu)
- ^ Sign up for The Conversation’s newsletter (theconversation.com)
- ^ Sitka, Alaska (www.rwjf.org)
- ^ rural infrastructure program (www.rd.usda.gov)
- ^ health-promoting activities (www.usda.gov)
- ^ demographics (doi.org)
- ^ politics (www.washingtonpost.com)
- ^ economics (www.census.gov)
- ^ Biden (www.nytimes.com)
Authors: Lauren Hughes, State Policy Director, Farley Health Policy Center; Associate Professor of Family Medicine, University of Colorado Anschutz Medical Campus

