How coronavirus contact tracing works in a state Dr. Fauci praised as a model to follow
- Written by Jenny Meredith, Clinical Assistant Professor of Pathology, University of South Carolina School of Medicine, University of South Carolina
After weeks of keeping people home to “flatten the curve[1],” restrictions on U.S. businesses are loosening and the coronavirus pandemic response is moving into a new phase.
Two things will be critical to keep COVID-19 cases from flaring up again: widespread testing to quickly identify anyone who gets the virus, and contact tracing to find everyone those individuals might have passed it to.
It’s a daunting task, but states are working hard to take the necessary steps to reopen safely. When Dr. Anthony Fauci, the head of the National Institute of Allergy and Infectious Disease, explained that task to the U.S. Senate[2] recently, he pointed to South Carolina as a model for the country, one that he would “almost like to clone.”
So, what is South Carolina getting right?
Part of it has to do with contact tracing. Since early March, when South Carolina’s first coronavirus case surfaced, investigators have reached out to every person who tested positive for SARS-CoV-2 in the state, and all of the people they came into close contact with[3]. To help prevent the virus from spreading farther, they hired 1,800 additional workers who will follow up with those contacts each day for 14 days to make sure they haven’t become ill.
Fauci’s compliment didn’t surprise me. I spent the first nine years of my career as a public health microbiologist in South Carolina at the Department of Health and Environmental Control’s State Public Health Laboratory. South Carolina already had disease reporting requirements in place and the cutting-edge laboratory technology needed for testing. Together with skilled epidemiologists, these laid the groundwork for an effective response[4] to a pandemic that, nationwide, has now claimed more than 100,000 U.S. lives[5].
Knowing where to look
The first step was scaling up testing – fast. To find and contain the virus, officials need to know where to look.
South Carolina is poised to conduct 220,000 tests[6] in May and June, close to the total for the previous three months combined, with a goal of testing 2% of the population. That’s still a low percentage, but it’s only an initial goal in the push to test more people. According to the Safra Center at Harvard University, testing between 2% and 6% of the population[7], coupled with effective contact tracing afterward, will be required to control the pandemic.
Partnering with private entities is an important part of how South Carolina has been able to ramp up testing and process those tests quickly. Prisma Health, the state’s largest health care system, and the Medical University of South Carolina have facilitated a large portion of the state’s testing, including providing the resources to collect thousands of samples at pop-up testing sites[8].
These community testing sites are initially focused on providing free screening and testing to underserved and rural communities across the state. The state is also working with partners across the state to provide testing for every nursing home resident[9] by the end of May.
Coronavirus contact tracing in action
What happens after the diagnosis is crucial for changing the course of the COVID-19 pandemic.
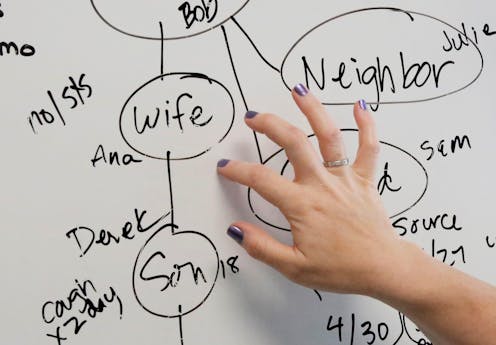
Once a positive case is identified, testing labs are required by law to report that patient’s contact information to the state health department. Case investigators then interview every person who tests positive for SARS-CoV-2, as they have been doing since the outbreak began.
These interviews can be lengthy, and they require staff with excellent interpersonal communication skills and training. The interviewers help patients recall their activities in the previous days and identify people they came in close contact with starting 48 hours before the onset of symptoms. Sometimes patients can’t recall specifics, or know only that they’ve been to a certain restaurant or event. In these cases, the investigation can take much longer as the health department tracks down event participants or alerts restaurant patrons that they may have been exposed when visiting during a particular time period.
The investigators also help patients understand what self-isolation means and what they’ll need to do to self-isolate for 10 days from the start of their symptoms.
The contacts who are identified during the case interview then go into a work queue for follow-up by contact tracers. Contact tracers want to reach these contacts before they spread the virus farther.
There isn’t much time. The respiratory symptoms of coronavirus take, on average, five to six days to appear[10], but they can take as long as 14 days, and a person can be shedding the virus during that time[11] and getting more people sick. Finding those people quickly and isolating them is critical. One study found undocumented infections caused about 80%[12] of China’s documented cases.
Following up every day with a ‘virtual handshake’
Tracers next alert these contacts that they may have been exposed to SARS-CoV-2 and advise them to self-quarantine for 14 days. This includes limiting their activities by staying home as much as possible and wearing a mask if they must go out.
Once fully staffed and adequately trained, contact tracers will follow up even more often, performing a “virtual handshake” with each identified contact every day for 14 days to ensure that those individuals are monitoring symptoms and taking precautions not to spread the illness. This could be a phone call or a quick text to check on symptoms.
In the future, contact tracing and follow-up could be performed digitally via cellphone apps[13] like those being used in other countries.
South Carolina was one of three states to announce on May 20 that they were partnering with Google and Apple[14] to develop ways to use new smartphone technology designed to quickly notify people when they have been exposed[15] to someone who has tested positive for the coronavirus. The technology has drawbacks, but it could provide quick notifications if people widely adopt it.
No matter the method, daily communication is key so state health officials know if that person becomes ill during the 14-day window. Testing can then be arranged and, if positive, the case investigators start the process again with a detailed interview to locate the next ring of contacts.
How many contact tracers are enough?
Contact tracing is an important piece of the puzzle to reopening the economy without triggering a spike in coronavirus cases and overwhelming the medical system.
The CDC and George Washington University recommend states have 30 tracers for every 100,000 residents[16]. South Carolina’s 1,800 contact tracers[17] meet that target. These tracers are a combination of newly hired Department of Health and Environmental Control staff and staff retained through private staffing companies. Members of the public have also expressed an interested in helping with contact tracing, and may be used if future need arises.
Will this workforce, coupled with an increase in test availability, be robust enough to contain a rebound in cases? This answer will depend on the responsiveness of public health authorities and the willingness of the citizens of the state to self-isolate and quarantine. Swift action by both will be needed to save lives.
[Get facts about coronavirus and the latest research. Sign up for The Conversation’s newsletter.[18]]
References
- ^ flatten the curve (theconversation.com)
- ^ explained that task to the U.S. Senate (www.help.senate.gov)
- ^ all of the people they came into close contact with (scdhec.gov)
- ^ effective response (scdhec.gov)
- ^ claimed more than 100,000 U.S. lives (coronavirus.jhu.edu)
- ^ poised to conduct 220,000 tests (scha.org)
- ^ testing between 2% and 6% of the population (ethics.harvard.edu)
- ^ pop-up testing sites (www.scdhec.gov)
- ^ every nursing home resident (scdhec.gov)
- ^ five to six days to appear (health.ucsd.edu)
- ^ be shedding the virus during that time (www.hopkinsguides.com)
- ^ undocumented infections caused about 80% (doi.org)
- ^ follow-up could be performed digitally via cellphone apps (www.nature.com)
- ^ partnering with Google and Apple (blog.google)
- ^ notify people when they have been exposed (theconversation.com)
- ^ 30 tracers for every 100,000 residents (www.cdc.gov)
- ^ 1,800 contact tracers (www.scdhec.gov)
- ^ Sign up for The Conversation’s newsletter. (theconversation.com)
Authors: Jenny Meredith, Clinical Assistant Professor of Pathology, University of South Carolina School of Medicine, University of South Carolina

