Why you should get a COVID-19 vaccine – even if you've already had the coronavirus
- Written by Jennifer T. Grier, Clinical Assistant Professor of Immunology,, University of South Carolina
A few weeks ago, a message popped up in the corner of my screen. “What do you think about people who have recently had COVID–19 getting the vaccine?” A friend of mine was eligible for a COVID–19 vaccine, but she had recently gotten over an infection with SARS–CoV–2. More people are becoming eligible for vaccines each week – including millions of people who have already recovered from a coronavirus infection[1]. Many are wondering whether they need the vaccine, especially people who have already been infected.
I study immune responses to respiratory infections[2], so I get a lot of these types of questions. A person can develop immunity – the ability to resist infection – from being infected with a virus or from getting a vaccine. However, immune protection isn’t always equal. The strength of the immune response, the length of time that the protection lasts and the variation of the immune response across people is very different between vaccine immunity and natural immunity for SARS–CoV–2. COVID–19 vaccines offer safer and more reliable immunity than natural infection.
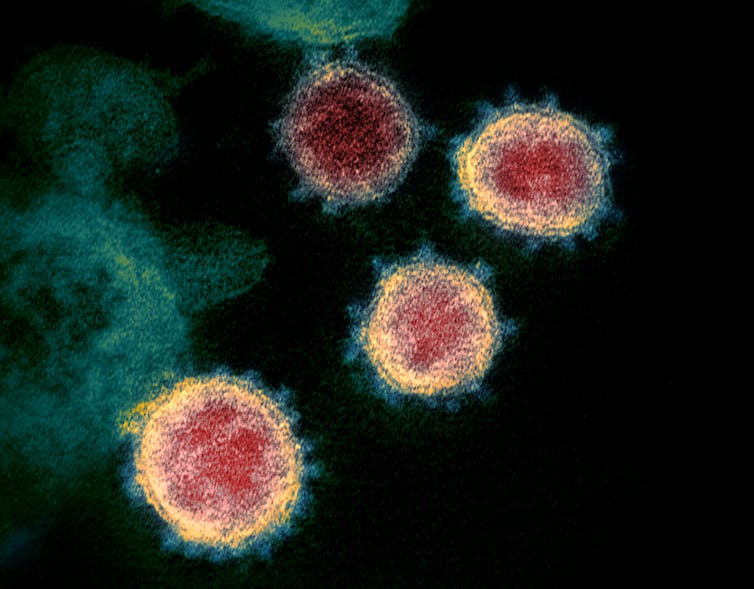 The immune system will usually generate an immune response to a SARS-CoV-2 infection, but not always.
National Institutes of Allergy and Infectious Diseases, CC BY[3][4]
The immune system will usually generate an immune response to a SARS-CoV-2 infection, but not always.
National Institutes of Allergy and Infectious Diseases, CC BY[3][4]
Immunity after infection is unpredictable
Immunity comes from the immune system’s ability to remember an infection. Using this immune memory, the body will know to fight if it encounters the disease again. Antibodies are proteins that can bind to a virus and prevent infection. T cells are cells that direct the removal of infected cells and viruses already bound by antibodies. These two are some of the main players that contribute to immunity.
After a SARS-CoV-2 infection, a person’s antibody and T cell responses may be strong enough to provide protection against reinfection[5]. Research shows that 91% of people who develop antibodies against the coronavirus are unlikely to be infected again for six months[6], even after a mild infection[7]. People who had no symptoms during the infection are also likely to develop immunity, though they tend to make fewer antibodies[8] than those who felt ill. So for some people, natural immunity may be strong and long-lasting.
The problem is that not everyone will develop immunity after a SARS-CoV-2 infection. As many as 9% of infected people do not have detectable antibodies[9], and up to 7% of people don’t have T cells that recognize the virus[10] 30 days after infection.
For people who do develop immunity, the strength and duration[11] of the protection can vary a lot. Up to 5% of people may lose their immune protection[12] within a few months. Without a strong immune defense, these people are susceptible to reinfection by the coronavirus. Some have had second bouts of COVID–19 as soon as one month after their first infection[13]; and, though rare, some people have been hospitalized or even died[14].
A person who is reinfected may also be able to transmit the coronavirus even without feeling sick[15]. This could put the person’s loved ones at risk.
And what about the variants? So far, there isn’t any hard data about the new coronavirus variants and natural immunity or reinfection, but it is certainly possible that immunity from one infection won’t be as strong against infection with a different variant.
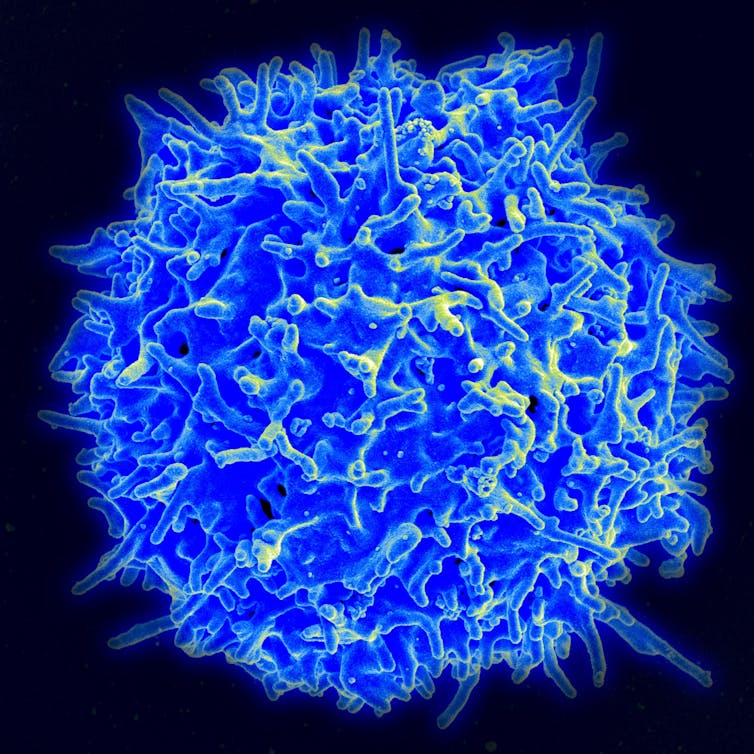 COVID–19 vaccines produce a strong immune response in terms of both antibodies and T cells, like the T cell in this photo.
National Institutes of Allergy and Infectious Diseases/National Institutes of Health[16]
COVID–19 vaccines produce a strong immune response in terms of both antibodies and T cells, like the T cell in this photo.
National Institutes of Allergy and Infectious Diseases/National Institutes of Health[16]
Vaccination leads to reliable protection
COVID–19 vaccines generate both antibody and T cell responses[17] – but this is much stronger and more consistent than immunity from natural infection. One study found that four months after receiving their first dose of the Moderna vaccine, 100% of people tested had antibodies against SARS-CoV-2[18]. This is the longest period that has been studied so far. In a study looking at the Pfizer and Moderna vaccines, antibody levels were also much higher in vaccinated people than in those who had recovered from infection[19].
Even better, a study in Israel[20] showed that the Pfizer vaccine blocked 90% of infections after both doses – even with a variant present in the population. And a decrease in infections[21] means people are less likely to transmit the virus to the people around them.
The COVID–19 vaccines aren’t perfect, but they produce strong antibody and T cell responses that offer a safer and more reliable means of protection than natural immunity.
Infection and vaccination together
To my friend’s message, I instantly replied that she should absolutely get the vaccine. After getting vaccinated, my friend could be comfortable knowing that she has long-lasting, effective immunity and less of a chance of spreading the coronavirus to her friends and family.
But more good news has emerged since I sent that message. A new study showed that vaccination after infection produces six times more antibodies[22] than a vaccine by itself. This isn’t to say that anyone should try to get infected before they get vaccinated – vaccine immunity alone is more than strong enough to provide protection and the dangers of a fight with COVID-19 far outweigh the benefits. But when my friend and the many others who were already infected get their vaccines, they’ll be well protected.
Natural immunity from infection is simply far too unreliable in the face of such a devastating virus. Current COVID-19 vaccines offer incredibly strong, consistent protection to the great majority of people. So, for anyone eligible, even those who have already had a SARS-CoV-2 infection, COVID-19 vaccines offer immense benefits.
[Get facts about coronavirus and the latest research. Sign up for The Conversation’s newsletter.[23]]
References
- ^ recovered from a coronavirus infection (www.cdc.gov)
- ^ I study immune responses to respiratory infections (scholar.google.com)
- ^ National Institutes of Allergy and Infectious Diseases (commons.wikimedia.org)
- ^ CC BY (creativecommons.org)
- ^ protection against reinfection (doi.org)
- ^ for six months (doi.org)
- ^ a mild infection (doi.org)
- ^ fewer antibodies (doi.org)
- ^ detectable antibodies (doi.org)
- ^ don’t have T cells that recognize the virus (doi.org)
- ^ strength and duration (doi.org)
- ^ lose their immune protection (doi.org)
- ^ one month after their first infection (doi.org)
- ^ hospitalized or even died (doi.org)
- ^ without feeling sick (doi.org)
- ^ National Institutes of Allergy and Infectious Diseases/National Institutes of Health (commons.wikimedia.org)
- ^ antibody and T cell responses (doi.org)
- ^ 100% of people tested had antibodies against SARS-CoV-2 (doi.org)
- ^ recovered from infection (doi.org)
- ^ study in Israel (doi.org)
- ^ decrease in infections (doi.org)
- ^ six times more antibodies (doi.org)
- ^ Sign up for The Conversation’s newsletter. (theconversation.com)
Authors: Jennifer T. Grier, Clinical Assistant Professor of Immunology,, University of South Carolina

