Is your neighborhood raising your coronavirus risk? Redlining decades ago set communities up for greater danger
- Written by Jeremy Németh, Associate Professor of Urban and Regional Planning, University of Colorado Denver
Vicente Arenas moved to the edge of Denver’s Valverde neighborhood, attracted by low housing prices and proximity to his downtown job just three miles away.
The 1-square-mile neighborhood mixes small, ranch-style homes with auto body shops, metal fabricators and industrial supply warehouses, and is hemmed in on its four sides by state highways and interstates. Much of Valverde is devoid of streetlights and wide sidewalks, a fact that Arenas laments. But he immediately felt a strong kinship with the local Hispanic population, which comprises 81% of residents[1].
“There is a real sense of familia in this area,” Arenas says, “where every house has multiple generations from the grandparents down to the little kids, families are piling into trucks together, and you’ll see five guys crowded around trying to fix an engine. And then there’s the smell of fresh tortillas every night.” The neighborhood is most vibrant in the evenings, he explains, when residents return home after long work days in the construction and food service industries.
But what makes Valverde so attractive to Arenas might also have raised its risks amid the coronavirus pandemic. Its location brings air pollution that can increase the risk of serious respiratory problems[2], bustling homes makes social distancing nearly impossible, and commuting together increases exposure to potentially infected individuals.
It came as little surprise to us, an urban planning professor[3] and infectious disease doctor[4], that Valverde had the highest COVID-19 hospitalization rate in the city[5].
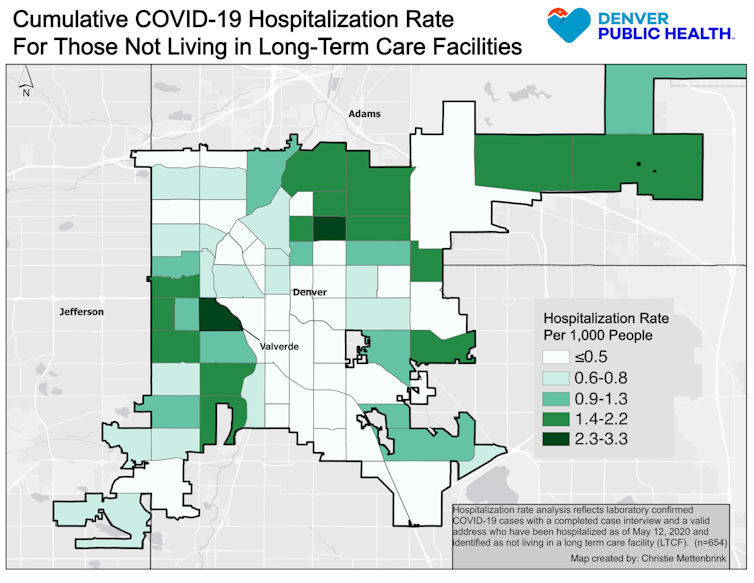 Denver Public Health[6]
Place matters
Public health officials and urban planners have long known that one’s ZIP code is an especially reliable indicator[7] of educational attainment, lifetime earnings and even life expectancy[8]. Near Washington, D.C., for example, residents of Chevy Chase can expect to live nearly 33 years longer[9] than those from Barry Farm, a neighborhood just 10 miles away.
ZIP code is also a great indicator of risk for disease transmission. Across the U.S., in cities as diverse as Austin[10], New York City[11] and San Francisco[12], lower-income communities of color are experiencing disproportionately high rates of COVID-19 infection, hospitalization and death.
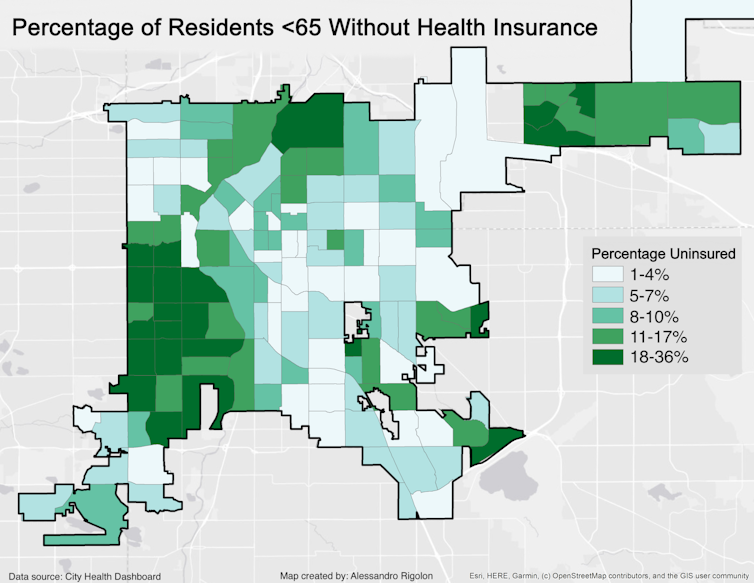
One set of explanations for these geographical disparities focuses on the individual circumstances of neighborhood residents. Indeed, for the 60% of low-wage U.S. workers[13] lucky enough to have kept their jobs through the crisis, those in “essential service” positions like construction, food preparation and retail cannot simply Zoom with colleagues from home[14]. They often rely on family members, who may themselves be in high-risk age groups, for child care and depend on crowded public transit[15] for their commutes before returning home to crowded apartments or houses[16]. And those with limited English fluency often struggle to obtain reliable health information[17]. Lacking health insurance often leads people to delay seeking medical care, sometimes resulting in severe health consequences.
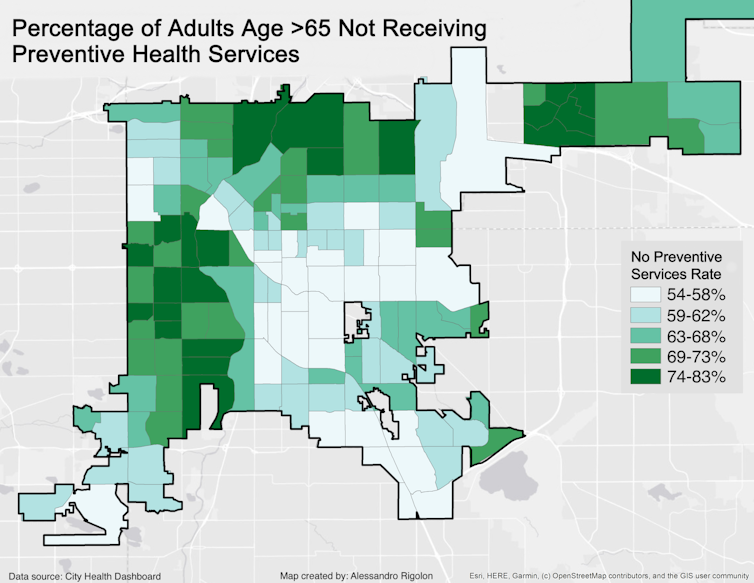
In Denver, neighborhood maps also reveal other influences. For example, maps of COVID-19 hospitalizations overlap with maps showing lack of health insurance[18] and access to preventive medical care[19].
Denver Public Health[6]
Place matters
Public health officials and urban planners have long known that one’s ZIP code is an especially reliable indicator[7] of educational attainment, lifetime earnings and even life expectancy[8]. Near Washington, D.C., for example, residents of Chevy Chase can expect to live nearly 33 years longer[9] than those from Barry Farm, a neighborhood just 10 miles away.
ZIP code is also a great indicator of risk for disease transmission. Across the U.S., in cities as diverse as Austin[10], New York City[11] and San Francisco[12], lower-income communities of color are experiencing disproportionately high rates of COVID-19 infection, hospitalization and death.
One set of explanations for these geographical disparities focuses on the individual circumstances of neighborhood residents. Indeed, for the 60% of low-wage U.S. workers[13] lucky enough to have kept their jobs through the crisis, those in “essential service” positions like construction, food preparation and retail cannot simply Zoom with colleagues from home[14]. They often rely on family members, who may themselves be in high-risk age groups, for child care and depend on crowded public transit[15] for their commutes before returning home to crowded apartments or houses[16]. And those with limited English fluency often struggle to obtain reliable health information[17]. Lacking health insurance often leads people to delay seeking medical care, sometimes resulting in severe health consequences.
In Denver, neighborhood maps also reveal other influences. For example, maps of COVID-19 hospitalizations overlap with maps showing lack of health insurance[18] and access to preventive medical care[19].
 Denver Public Health[20]
Denver Public Health[20]
 Denver Public Health[21]
Yet few people have focused on how neighborhood characteristics, or environmental factors[22], might play a role in virus transmission. Is it possible that neighborhoods themselves are making people sick[23]?
It’s likely. The CDC says[24] that people with asthma are at higher risk for severe illness if they contract COVID-19, and rates of asthma are notoriously elevated near highways[25] like those surrounding Valverde. Diabetes[26], hypertension[27] and obesity[28] rates are also strong risk factors for virus contraction; these conditions are linked to physical activity and diet, which are themselves directly influenced by access to quality walking and biking infrastructure[29], parks[30] and healthy food outlets[31], all features that tend to be lacking in disadvantaged neighborhoods.
The legacy of redlining
Why does this geographical clustering of disadvantage and privilege occur in cities around the U.S.?
Much of our present-day disparities in health, wealth and social mobility can be traced back to the 1930s, when Valverde and similar neighborhoods were “redlined[32]” by the Home Owner’s Loan Corporation. In this racist practice[33], banks drew red lines on a map around neighborhoods with populations of color, restricting lending in these places and starving them of investment for generations to come.
Denver Public Health[21]
Yet few people have focused on how neighborhood characteristics, or environmental factors[22], might play a role in virus transmission. Is it possible that neighborhoods themselves are making people sick[23]?
It’s likely. The CDC says[24] that people with asthma are at higher risk for severe illness if they contract COVID-19, and rates of asthma are notoriously elevated near highways[25] like those surrounding Valverde. Diabetes[26], hypertension[27] and obesity[28] rates are also strong risk factors for virus contraction; these conditions are linked to physical activity and diet, which are themselves directly influenced by access to quality walking and biking infrastructure[29], parks[30] and healthy food outlets[31], all features that tend to be lacking in disadvantaged neighborhoods.
The legacy of redlining
Why does this geographical clustering of disadvantage and privilege occur in cities around the U.S.?
Much of our present-day disparities in health, wealth and social mobility can be traced back to the 1930s, when Valverde and similar neighborhoods were “redlined[32]” by the Home Owner’s Loan Corporation. In this racist practice[33], banks drew red lines on a map around neighborhoods with populations of color, restricting lending in these places and starving them of investment for generations to come.
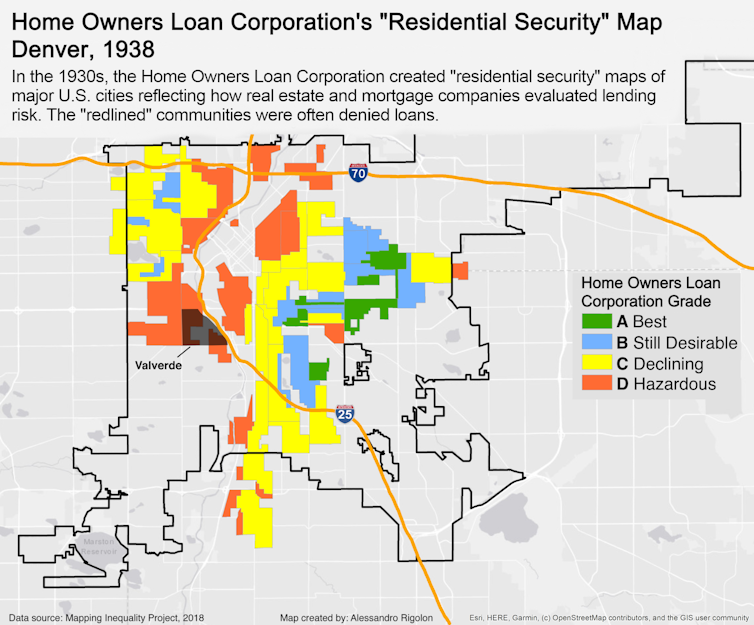 Mapping Inequality Project, CC BY-NC-SA[34][35]
The legacies of redlining are well-documented. Due to decades of disinvestment, once-redlined neighborhoods[36] have higher poverty rates[37], lower-performing schools[38], more segregation[39], lower social mobility[40], greater exposure to extreme heat[41], fewer parks[42], higher gentrification rates[43], and more indicators of urban decline[44] than those that were not. Property is also the primary way that families build and inherit wealth in America; the average white family now holds 10 times the wealth[45] of the average black family and seven times the average Hispanic family.
In Denver, decades of legally sanctioned disinvestment and segregation made redlined neighborhoods fertile ground for the siting of polluting industrial facilities[46] and two interstate highways, one of which runs directly through Valverde – a familiar story in cities around the U.S.[47].
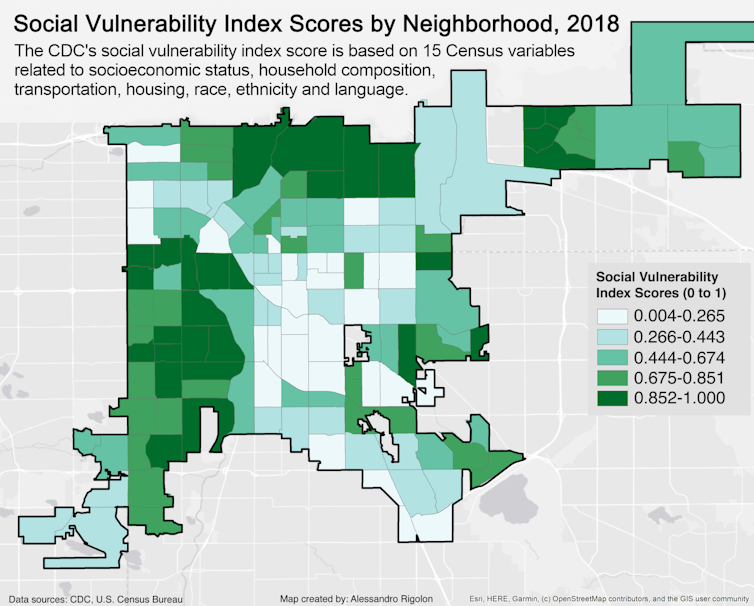
These inequities have contributed to vast differences in levels of social vulnerability[48] – the constellation of individual and environmental circumstances that weaken a community’s ability to prepare for and respond to crises like this pandemic. Mapping scores on the CDC’s Social Vulnerability Index[49] in Denver reveals how these clear patterns of disadvantage[50] coincide with COVID-19 hospitalization rates.
Mapping Inequality Project, CC BY-NC-SA[34][35]
The legacies of redlining are well-documented. Due to decades of disinvestment, once-redlined neighborhoods[36] have higher poverty rates[37], lower-performing schools[38], more segregation[39], lower social mobility[40], greater exposure to extreme heat[41], fewer parks[42], higher gentrification rates[43], and more indicators of urban decline[44] than those that were not. Property is also the primary way that families build and inherit wealth in America; the average white family now holds 10 times the wealth[45] of the average black family and seven times the average Hispanic family.
In Denver, decades of legally sanctioned disinvestment and segregation made redlined neighborhoods fertile ground for the siting of polluting industrial facilities[46] and two interstate highways, one of which runs directly through Valverde – a familiar story in cities around the U.S.[47].
These inequities have contributed to vast differences in levels of social vulnerability[48] – the constellation of individual and environmental circumstances that weaken a community’s ability to prepare for and respond to crises like this pandemic. Mapping scores on the CDC’s Social Vulnerability Index[49] in Denver reveals how these clear patterns of disadvantage[50] coincide with COVID-19 hospitalization rates.
 CDC, U.S. Census Bureau, CC BY-SA[51][52]
Building healthier cities
Given these realities, how can cities best contain this virus and plan for the next pandemic?
A decentralized, health equity-oriented approach[53] to fighting the epidemic that brings testing and support services into our most historically vulnerable neighborhoods can increase access to preventive health care and improve health[54] across entire communities.
In the short term, critical efforts can include widespread free testing events in vulnerable neighborhoods, along with distribution of free hand sanitizer, cleaning supplies and masks, which also helps ensure that at-risk residents do not have to travel on crowded public transportation to shop for these items. This is also an opportunity to link uninsured residents to health care coverage and primary care providers.
Denver Mayor Michael Hancock recently said the city is committed to “taking the test to the people[55], particularly where our most vulnerable residents live.” And in April, San Francisco rolled out temporary field care clinics[56] in at-risk neighborhoods. Health care workers in these dispersed clinics are trained to provide culturally and linguistically appropriate medical information about what to do if one feels sick, what testing and treatment options exist and how to prevent further spread of COVID-19.
In the longer term, urban planners have demonstrated how a commitment to building healthy urban environments[57] – those that prioritize walking and cycling, promote recreation, produce more affordable housing, allow residents to access healthy food locally and provide public transportation options – can have long-lasting impacts for all residents.
In addition, locating neighborhood health centers[58] in at-risk neighborhoods has been proven to improve health and build a sense of community trust that can be instrumental in times of crisis.
America is at a crossroads, and cities can embrace this opportunity to address health disparities. Health care officials and urban planning professionals are beginning to work together to help lift communities[59] from the legacy of discriminatory policies. By employing interventions that acknowledge the power of place, the country can mitigate harm from the current epidemic and help create more just, healthy and resilient communities that are better prepared for future challenges.
CDC, U.S. Census Bureau, CC BY-SA[51][52]
Building healthier cities
Given these realities, how can cities best contain this virus and plan for the next pandemic?
A decentralized, health equity-oriented approach[53] to fighting the epidemic that brings testing and support services into our most historically vulnerable neighborhoods can increase access to preventive health care and improve health[54] across entire communities.
In the short term, critical efforts can include widespread free testing events in vulnerable neighborhoods, along with distribution of free hand sanitizer, cleaning supplies and masks, which also helps ensure that at-risk residents do not have to travel on crowded public transportation to shop for these items. This is also an opportunity to link uninsured residents to health care coverage and primary care providers.
Denver Mayor Michael Hancock recently said the city is committed to “taking the test to the people[55], particularly where our most vulnerable residents live.” And in April, San Francisco rolled out temporary field care clinics[56] in at-risk neighborhoods. Health care workers in these dispersed clinics are trained to provide culturally and linguistically appropriate medical information about what to do if one feels sick, what testing and treatment options exist and how to prevent further spread of COVID-19.
In the longer term, urban planners have demonstrated how a commitment to building healthy urban environments[57] – those that prioritize walking and cycling, promote recreation, produce more affordable housing, allow residents to access healthy food locally and provide public transportation options – can have long-lasting impacts for all residents.
In addition, locating neighborhood health centers[58] in at-risk neighborhoods has been proven to improve health and build a sense of community trust that can be instrumental in times of crisis.
America is at a crossroads, and cities can embrace this opportunity to address health disparities. Health care officials and urban planning professionals are beginning to work together to help lift communities[59] from the legacy of discriminatory policies. By employing interventions that acknowledge the power of place, the country can mitigate harm from the current epidemic and help create more just, healthy and resilient communities that are better prepared for future challenges.
References
- ^ which comprises 81% of residents (www.denvergov.org)
- ^ increase the risk of serious respiratory problems (projects.iq.harvard.edu)
- ^ urban planning professor (jeremynemeth.com)
- ^ infectious disease doctor (www.denverhealth.org)
- ^ the highest COVID-19 hospitalization rate in the city (storymaps.arcgis.com)
- ^ Denver Public Health (www.denverpublichealth.org)
- ^ one’s ZIP code is an especially reliable indicator (www.opportunityatlas.org)
- ^ life expectancy (www.nytimes.com)
- ^ 33 years longer (www.washingtonpost.com)
- ^ Austin (sph.uth.edu)
- ^ New York City (covid19tracker.health.ny.gov)
- ^ San Francisco (www.cdph.ca.gov)
- ^ 60% of low-wage U.S. workers (www.federalreserve.gov)
- ^ cannot simply Zoom with colleagues from home (www.epi.org)
- ^ depend on crowded public transit (www.governing.com)
- ^ crowded apartments or houses (www.ppic.org)
- ^ struggle to obtain reliable health information (dx.doi.org)
- ^ health insurance (www.kff.org)
- ^ access to preventive medical care (www.cityhealthdashboard.com)
- ^ Denver Public Health (www.denverpublichealth.org)
- ^ Denver Public Health (www.denverpublichealth.org)
- ^ environmental factors (www.ncbi.nlm.nih.gov)
- ^ are making people sick (www.urban.org)
- ^ CDC says (www.cdc.gov)
- ^ notoriously elevated near highways (doi.org)
- ^ Diabetes (doi.org)
- ^ hypertension (doi.org)
- ^ obesity (doi.org)
- ^ quality walking and biking infrastructure (doi.org)
- ^ parks (doi.org)
- ^ healthy food outlets (doi.org)
- ^ redlined (dsl.richmond.edu)
- ^ In this racist practice (dsl.richmond.edu)
- ^ Mapping Inequality Project (dsl.richmond.edu)
- ^ CC BY-NC-SA (creativecommons.org)
- ^ once-redlined neighborhoods (dsl.richmond.edu)
- ^ higher poverty rates (www.citylab.com)
- ^ lower-performing schools (www.epi.org)
- ^ more segregation (www.epi.org)
- ^ lower social mobility (opportunityinsights.org)
- ^ greater exposure to extreme heat (doi.org)
- ^ fewer parks (doi.org)
- ^ higher gentrification rates (denverite.com)
- ^ more indicators of urban decline (journals.sagepub.com)
- ^ 10 times the wealth (www.brookings.edu)
- ^ siting of polluting industrial facilities (www.attomdata.com)
- ^ in cities around the U.S. (www.theatlantic.com)
- ^ social vulnerability (svi.cdc.gov)
- ^ CDC’s Social Vulnerability Index (svi.cdc.gov)
- ^ these clear patterns of disadvantage (denverite.com)
- ^ CDC, U.S. Census Bureau (svi.cdc.gov)
- ^ CC BY-SA (creativecommons.org)
- ^ health equity-oriented approach (www.apha.org)
- ^ increase access to preventive health care and improve health (www.kff.org)
- ^ taking the test to the people (denverite.com)
- ^ temporary field care clinics (sfmayor.org)
- ^ building healthy urban environments (theconversation.com)
- ^ neighborhood health centers (www.hrsa.gov)
- ^ to help lift communities (www.acheinc.org)
Authors: Jeremy Németh, Associate Professor of Urban and Regional Planning, University of Colorado Denver

